Vol No: 5 Issue No: 3 eISSN:
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Dr. Dhanya V, Assistant Professor, Department of Pathology, KMCT Medical College, Manassery, Kerala, India.
2Department of Pathology, KMCT Medical College, Manassery, Kerala, India
3Department of Gastroenterology, KMCT Medical College, Manassery, Kerala, India
4Department of Gastroenterology, National Hospital, Kozhikode, Kerala, India
5Department of Pathology, KMCT Medical College, Manassery, Kerala, India
*Corresponding Author:
Dr. Dhanya V, Assistant Professor, Department of Pathology, KMCT Medical College, Manassery, Kerala, India., Email: pcdhanyanair@gmail.com
Abstract
Background: Upper gastrointestinal endoscopy with biopsy is a widely used diagnostic procedure for patients presenting with dyspepsia and abdominal pain. Persistent or recurrent symptoms often cause significant discomfort, making endoscopy an essential component of patient care. Histopathological evaluation of biopsies helps detect mucosal abnormalities and confirm clinical diagnoses.
Objectives: To correlate clinical, endoscopic, and histopathological findings of gastric biopsies received in the Department of Pathology.
Methods: A retrospective cross-sectional study was conducted on adequately sampled gastric mucosal biopsies over four years. Clinical, endoscopic, and histopathological data were compiled and analyzed to establish correlations.
Results: A total of 821 gastric biopsies were analyzed, predominantly from the antrum. Patient age ranged from 12-80 years, with a slight male predominance (54%). Dyspepsia (26.4%) and abdominal discomfort (24.7%) were the most common complaints. Endoscopic findings included erythema (52.6%) and ulceration (22.8%). Chronic gastritis was the predominant histopathological diagnosis (91.9%), with Helicobacter pylori detected in 25.7% of cases. Gastric malignancy was identified in 5.1% of biopsies. Correlation between clinical and endoscopic findings, as well as between endoscopic and histopathological findings, was statistically significant (P < 0.0001).
Conclusion: The present study demonstrated strong correlations between clinical, endoscopic, and histopathological findings. Endoscopy combined with biopsy remains vital for accurate diagnosis and effective management of gastrointestinal symptoms. Random biopsies in symptomatic patients, even without significant endoscopic changes, can yield important diagnostic insights and guide appropriate clinical management.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Upper gastrointestinal (GI) disorders are among the most common presenting complaints in outpatient departments. Their prevalence in the general population is high and they contribute significantly to morbidity.1,2 Upper endoscopy has become a valuable tool in theevaluation of gastrointestinal symptoms.3 It employs aevaluation of gastrointestinal symptoms.3 It employs a lighted, flexible fiberoptic or video endoscope for visualization of the upper gastrointestinal tract.4 The decision to obtain a biopsy depends on the patient’s specific symptoms and any structural architecture or abnormal findings observed during endoscopic evaluation by a gastroenterologist. Gastric biopsy specimens obtained through endoscopy are examined by a qualified pathologist, and the results play a crucial role in guiding the appropriate management of patients with gastrointestinal symptoms.5
Hence, upper GI endoscopy serves as the first-line investigation in the workup of patients presenting with dyspeptic symptoms. Findings on upper gastrointestinal endoscopy are variable. Gastritis is the most common finding, accounting for nearly half of the cases, as reported by Dhungana D et al.6 Other frequent findings include duodenal and gastric ulcers. The prevalence of Helicobacter pylori infection in India is high (49.94%-83.30%), yet the incidence of gastric cancer remains comparatively low, suggesting a complex association between H. pylori infection and gastric cancer.7 Approximately 2.4% of patients undergoing diagnostic endoscopy are diagnosed with gastric cancer, which may be attributed to the high prevalence of H. pylori infection and chronic atrophic gastritis in the Indian population.8 Therefore, early detection of H. pylori infection and gastric cancer is essential for effective management and improved patient survival. The changing trends in the presentation, prevalence, and morphology of gastrointestinal disorders are noteworthy. In this study, we aimed to correlate the clinical, endoscopic, and histopathological findings of gastric biopsies obtained during endoscopy.
Materials and Methods
The present study was a retrospective cross-sectional study conducted in the Department of Pathology, KMCT Medical College, Mukkam, Kozhikode, Kerala, over a period of four years from June 2020 to June 2024.
Inclusion Criteria
All gastric biopsy specimens, excluding those obtained from polyps or growths, received in the department during the study period.
Exclusion Criteria
1. Gastric biopsies obtained from endoscopically evident growths/polyps.
2. Inadequate biopsy samples showing only fibro-collagenous tissue or inflammatory exudates.
The clinical history provided in the request forms and medical records was reviewed, and the corresponding endoscopic findings were duly noted. Biopsy specimens were received in 10% neutral buffered formalin, and tissue bits were embedded in paraffin blocks. Three serial sections were prepared and stained with hematoxylin and eosin (H&E). Additional sections were stained with Giemsa stain for the detection of H. pylori. Neoplastic lesions were classified according to the World Health Organization (WHO) classification of tumors.9
Statistical Analysis
This was a descriptive study conducted to correlate age, gender, clinical features, and endoscopic findings with the final histopathological diagnoses. The data collected were analyzed to determine the percentage of concordance between endoscopic and histopathological findings. All data were compiled in Microsoft Excel and analyzed using Statistical Package for the Social Sciences (SPSS) software.
Results
A total of 821 gastric biopsy specimens were received during the study period. The majority of biopsies were obtained from the antrum (81.6%), followed by the body (9.5%), fundus (3.3%), pylorus (0.5%), pan-gastric sites (0.5%), duodenum (0.6%). Non-specified sites accounted for 4% of the biopsies.
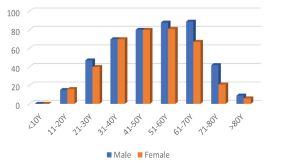
The age of the patients ranged from 12 to 80 years, with most cases occurring in individuals aged 41-70 years. Males constituted approximately 54% of the study population (Figure1).
The most common presenting complaints were dyspepsia (26.4%), abdominal discomfort (25%), and abdominal pain (24.7%). Many patients reported a combination of symptoms, most frequently the concurrence of dyspepsia and abdominal discomfort. Other noticeable presentations included heartburn, bloating, vomiting, and loss of weight. A smaller number of patients were referred for evaluation of anemia, upper GI bleed, or melena.
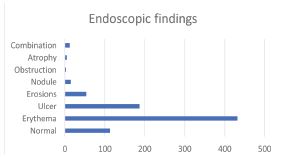
Among endoscopic findings, erythema was the most common observation (52.6%), followed by ulcers (22.8%) and erosions (6.6%). Approximately 13.8% of cases showed no detectable mucosal changes on endoscopy (Figure 2). The clinical presentations were correlated with endoscopic findings, and the association was found to be statistically significant (P <0.0001) (Table 1).
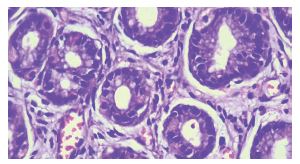
The most common histopathological diagnosis was chronic gastritis, accounting for 91.9% of cases (Figure 3). Approximately 5.1% of biopsies were diagnosed as gastric malignancy, the most frequent histological subtype being signet-ring carcinoma. Dysplasia without any clinical suspicion of malignancy was observed in 0.8% of cases, while atrophic gastritis was identified in 0.6%. Chronic gastritis was associated with additional pathological findings such as activity (3%), intestinal metaplasia (1.8%), and ulceration (0.5%).
The correlation between endoscopic findings and histopathological findings was statistically significant (P <0.0001) (Table 2).
Discussion
Gastrointestinal symptoms like heart burn, abdominal pain, and bloating are among the most common presenting complaints in outpatient departments. Recurring symptoms often cause considerable discomfort and concern for patients and are a major reason for referral to gastroenterology department. Clinical evaluation and endoscopy have become routine diagnostic interventions in tertiary care centers.
Over the past few decades, endoscopic procedures have undergone remarkable technological advancements-from the use of rigid hollow metal tubes to the development of lightweight, flexible fiber-optic endoscopes with illumination. Endoscopy not only enables direct visualization of GI tract but also facilitates targeted biopsies from suspected lesions. Thus, endoscopy combined with biopsy serves as an effective and cost-efficient minimally invasive approach for establishing specific diagnosis of patients with gastrointestinal disorders.
This study included all gastric biopsy specimens obtained through endoscopic procedures performed for patients presenting with GI symptoms. Endoscopically detected polypoidal lesions and growths were excluded from the analysis. A total of 821 cases were received in the Department of Pathology over a period of four years.
Most common symptoms noted in the present study included dyspepsia (26.7%), abdominal discomfort (25%), abdominal pain (24.7%), and heartburn (19.4%). These findings are comparable to those reported by Shanmugasamy et al., and Pruthi S et al., who also identified dyspepsia as the predominant symptom. However, our results differ from those of Godkhindi V et al., Khand-elia R et al., and Sharma A et al., in which abdominal pain was the most common reported symptom.9,10,11,12,13
In the present study, the most frequent site of gastric biopsy was the antrum (66.5%), followed by the body and fundus. Occasionally, pangastric biopsies were performed in cases where no obvious lesion was detected on endoscopy.3,14,15
The age of the patients ranged from 12 to 80 years, with the majority belonging to the 41-70-year age group (41%). Males constituted about 54% of the study population. These findings are consistent with those reported by Sharma A et al., and Godkhindi V et al.13,11
The most common presenting complaints were dyspepsia (26.4%), abdominal discomfort (25%), and abdominal pain (24.7%). Many patients presented with a combination of symptoms, predominantly dyspepsia and abdominal discomfort. These findings are similar to those reported by Khandelia R et al., and Sharma A et al.12,13
Among the endoscopic findings, erythema was the most common observation (52.6%), followed by ulcers (22.8%), and erosions (6.6%). About 13.8% cases showed normal endoscopy findings. The clinical presentations were correlated with endoscopic findings, and the association was found to be statistically significant (P <0.0001). The results of this study are consistent with those reported by Khandelia R et al., and Sharma A et al., but differ from the findings of Okoye OG et al.12,13,16
Histopathological examination remains the gold standard test for diagnosing and managing patients with recurrent gastrointestinal symptoms. In the present study, the majority of cases were diagnosed as chronic gastritis, accounting for 91.9% of the study population.H. pylori-induced chronic gastritis was the most common histological finding, observed in 25.7% of cases. Chronic gastritis was associated with additional pathological findings like activity (3%), intestinal meta-plasia (1.8%), and ulceration (0.5%). Approximately 5.1% of biopsies were diagnosed as gastric malignancy, while 0.8% showed dysplasia without any clinical suspicion of malignancy. The most common histological sub-type of malignancy was signet-ring carcinoma. Atrophic gastritis was identified in 0.6% of cases. These findings are consistent with those reported by Sharma et al., Malik MF et al., and Amin K et al.13,14,17
The endoscopic findings were correlated with the corresponding histopathological findings, and the association was found to be statistically significant (P <0.0001). The results of the present study are consistent with those reported by Grace H Elta et al., Pailoor K et al., but differ from the observations of Sharma S et al., and Poudel A et al.18,19,20,21
Conclusion
In conclusion, this study demonstrated a strong correla-tion between clinical and endoscopic findings as well as significant association between endoscopic findings and the final histopathological diagnoses. The most common pathological finding was chronic gastritis, with Helicobacter pylori identified as the predominant etiological factor. Significant pathological changes were detected in patients with gastrointestinal symptoms despite normal endoscopic findings. The practice of obtaining biopsies in such patients proved valuable, revealing pathologic conditions such as H. pylori infection, chronic gastritis, and gastric atrophy. These results emphasize the critical role of histopathologic evaluation in the management of patients with gastrointestinal symptoms. To conclude, combined use of endoscopy and biopsy represent a powerful tool in the diagnosis and treatment of patients with gastrointestinal disorders.
Conflict of Interest
There are no conflicts of interest
Acknowledgement
We would like to thank the laboratory staff and tech-nicians of KMCT Medical College for the cooperation during the study period
Supporting File
References
1. Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology 2006;130(5):1466-1479.
2. Kurata JH, Nogawa AN, Everhart JE. A prospective study of dyspepsia in primary care. Dig Dis Sci 2002;47(4):797-803.
3. Teriaky A, AlNasser A, McLean C, et al. The utility of endoscopic biopsies in patients with normal upper endoscopy. Can J Gastroenterol Hepatol 2016;2016:3026563.
4. Olokoba AB, Bojuwoye BJ, Yusuf M, et al. Common indications for upper gastro-intestinal tract end oscopy in ECWA Hospital, Egbe, Nigeria: A preliminary report. Afr Sci 2006;7(4):165-9.
5. Lazenby AJ. Gastroenterologist/pathologist partnership. Tech Gastrointest Endosc 2002;4(2):95-100.
6. Dhungana D, Regmi YN. Prevalence of gastritis in a tertiary care centre: A descriptive cross-sectional study. JNMA J Nepal Med Assoc 2021; 59(234):120-123.
7. Misra V, Pandey R, Misra SP, et al. Helicobacter pylori and gastric cancer: Indian enigma. World J Gastroenterol 2014;20(6):1503-9.
8. Mohapatra A, Mohapatra S, Mahawar S, et al. Endoscopic diagnosis and prevalence of early gastric cancer in India: A prospective study. DEN Open 2023;4(1):e309.
9. Shanmugasamy K, Bhavani K, Vaithy AK, et al. Clinical correlation of upper gastrointestinal end-oscopic biopsies with histopathological findings and to study the histopathological profile of various neoplastic and non-neoplastic lesions. Journal of Pharmaceutical and Biomedical Sciences 2016;6(4):2230-7885.
10. Pruthi S, Nirupama M, Chakraborti S. Evaluation of gastric biopsies in chronic gastritis: Grad-ing of inflammation by Visual Analogue Scale. Medical Journal of Dr. D.Y. Patil University. 2014;7(4):463-467.
11. Godkhindi V. The histopathological study of various gastro-duodenal lesions and their association with Helicobacter pylori infection. IOSR Journal of Dental and Medical Sciences. 2013;4:51-55.
12. Khandelia R, Saikia M. Histopathologic spectrum of upper gastrointestinal tract mucosal biopsies: A prospective study. International Journal of Medical Science and Clinical Invention 2017;4(11): 3314-3316.
13. Sharma A, Gupta K. Clinicopathological correlation of upper gastrointestinal tract endoscopic biopsies in a tertiary care hospital in rural area of North India. International Journal of Advanced Research 2020;8(3):1155-1160.
14. Amin K, Alam Z, Nagra MH, et al. Association of Helicobacter pylori with non-ulcer dyspepsia. Prof Med J 2003;10(3):11.
15. Nwokediuko SC, Okafor OC. Gastric Mucosa In Non-ulcer Dyspepsia: A histopathological study of Nigerian patients. Internet J Gastroenterol 2006;5(2):1-6.
16. Okoye OG, Olaomi OO, Nwofor AM, et al. Correlation of clinical, endoscopic, and patholo-gical findings among suspected peptic ulcer disease patients in Abuja, Nigeria. Gastroenterol Res Pract 2021;2021:9646932.
17. Malik MF, Hussain T, Khan MN, et al. Helicobacter pylori infection in patients with dyspeptic symp-toms having normal endoscopy. Pak Armed Forces Med J 2010;60(1):8.
18. Elta GH, Appelman HD, Behler EM, et al. A study of the correlation between endoscopic and histological diagnoses in gastroduodenitis. Am J Gastroenterol 1987;82(8):749-753.
19. Pailoor K, Sarpangala MK, Naik RCN. Histopathological diagnosis of gastric biopsies in correlation with endoscopy - A study in a tertiary care center. Advance Laboratory Medicine International 2012;3(2):22-31.
20. Sharma S, Makaju R, Dhakal R, et al. Correlation between endoscopic and histopathological findings in gastric lesions. Kathmandu Univ Med J (KUMJ) 2015;13(51):216-219.
21. Poudel A, Regmi S, Poudel S, et al. Correlation between endoscopic and histopathological findings in gastric lesions. Journal of Universal College of Medical Sciences 2013;1(3):37-41.